IMMUNISATION
How Immunisation Protects Us
What is Immunisation?
Immunisation is the process of using a vaccine to make a person immune to a specific disease. It's a key part of protecting our community's health, and it works by teaching your body how to fight off certain diseases. This simple act of prevention is considered one of the most significant medical advancements in history, saving countless lives and protecting generations from suffering.
The Power of Prevention
Immunisation is crucial for public health because it prevents the spread of diseases and reduces the strain on our healthcare system. It's a proactive way to stop outbreaks before they gain momentum. Since vaccinations were introduced in Australia in 1932, there has been a 99% decrease in deaths caused by vaccine-preventable diseases. While many of these diseases may seem like a thing of the past, outbreaks can still occur when a community's immunity wanes.
How Vaccines Work
Think of a vaccine as a "wanted" poster for your immune system. Vaccines contain a small, modified part of a germ (like a virus or bacteria). This antigen is not strong enough to make you sick, but it's enough to get your immune system's attention. When you get a vaccine, your body recognises the antigen and learns how to build a defense against it. If you ever encounter the real disease, your immune system will remember it and be able to fight it off quickly and effectively before it can cause serious harm.
A Foundation of Safety and Trust
We understand that questions about vaccine safety are important. You can be assured that vaccines are some of the most studied and rigorously tested medications in the world. Before a vaccine is made available in Australia, it must pass extremely strict and robust testing and registration programs. The Australian Government's Therapeutic Goods Administration (TGA) is responsible for this rigorous testing and ongoing monitoring, with a process that can take up to 20 years.
We are committed to addressing vaccine misinformation and fear-mongering by providing evidence-based, accurate information. While it is possible to experience mild side effects like a sore arm or a slight fever, serious adverse reactions are extremely rare.
Our Role: Your Trusted Guide
The Immunisation Foundation of Australia (IFA) is your community-driven guide to immunisation. While government bodies like the Department of Health manage the official National Immunisation Program, we focus on empowering the community. We combine powerful personal stories from families affected by vaccine-preventable diseases with credible scientific information to help you understand the critical role of immunisation in protecting our collective health.
Who Can be Immunised?
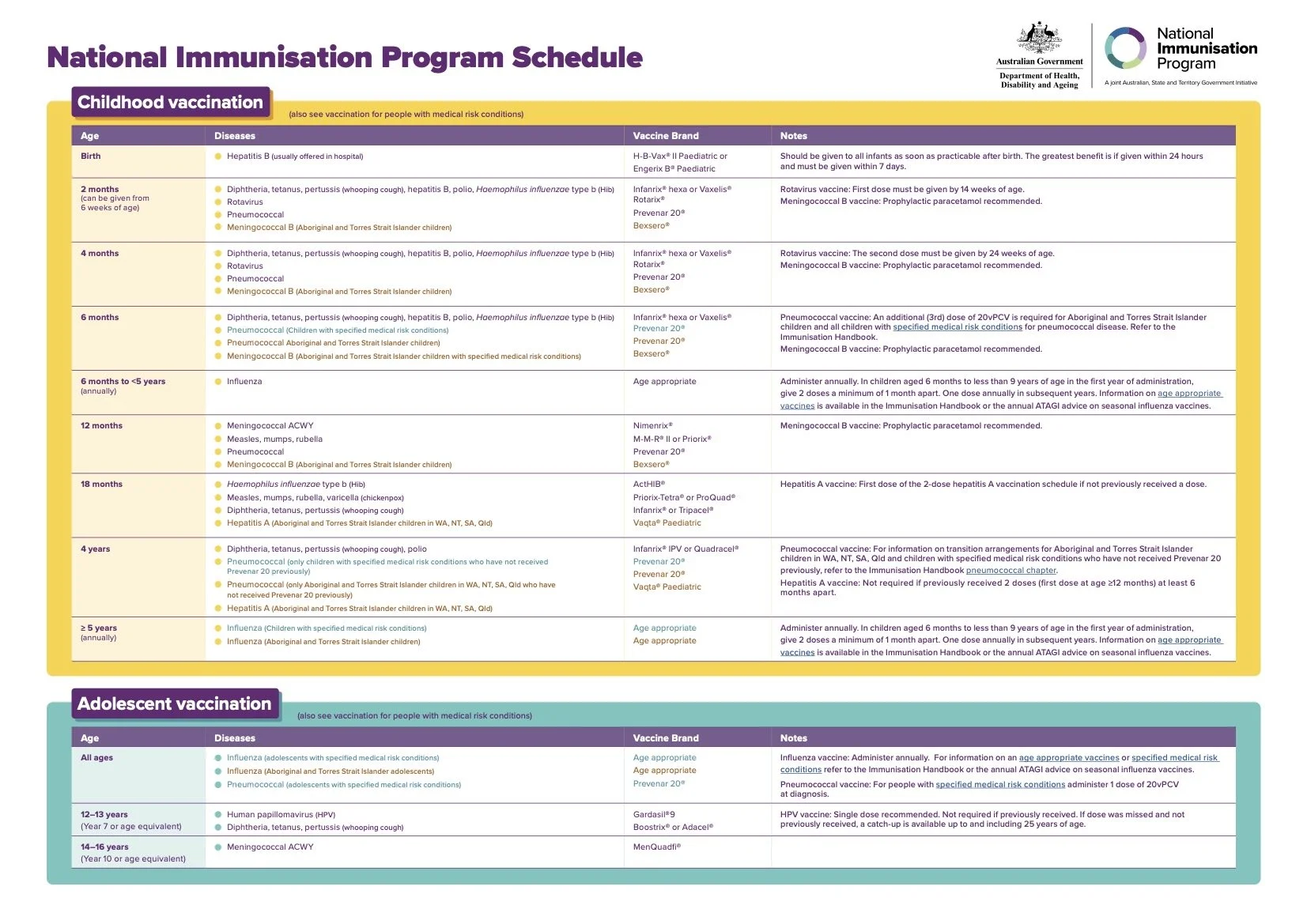
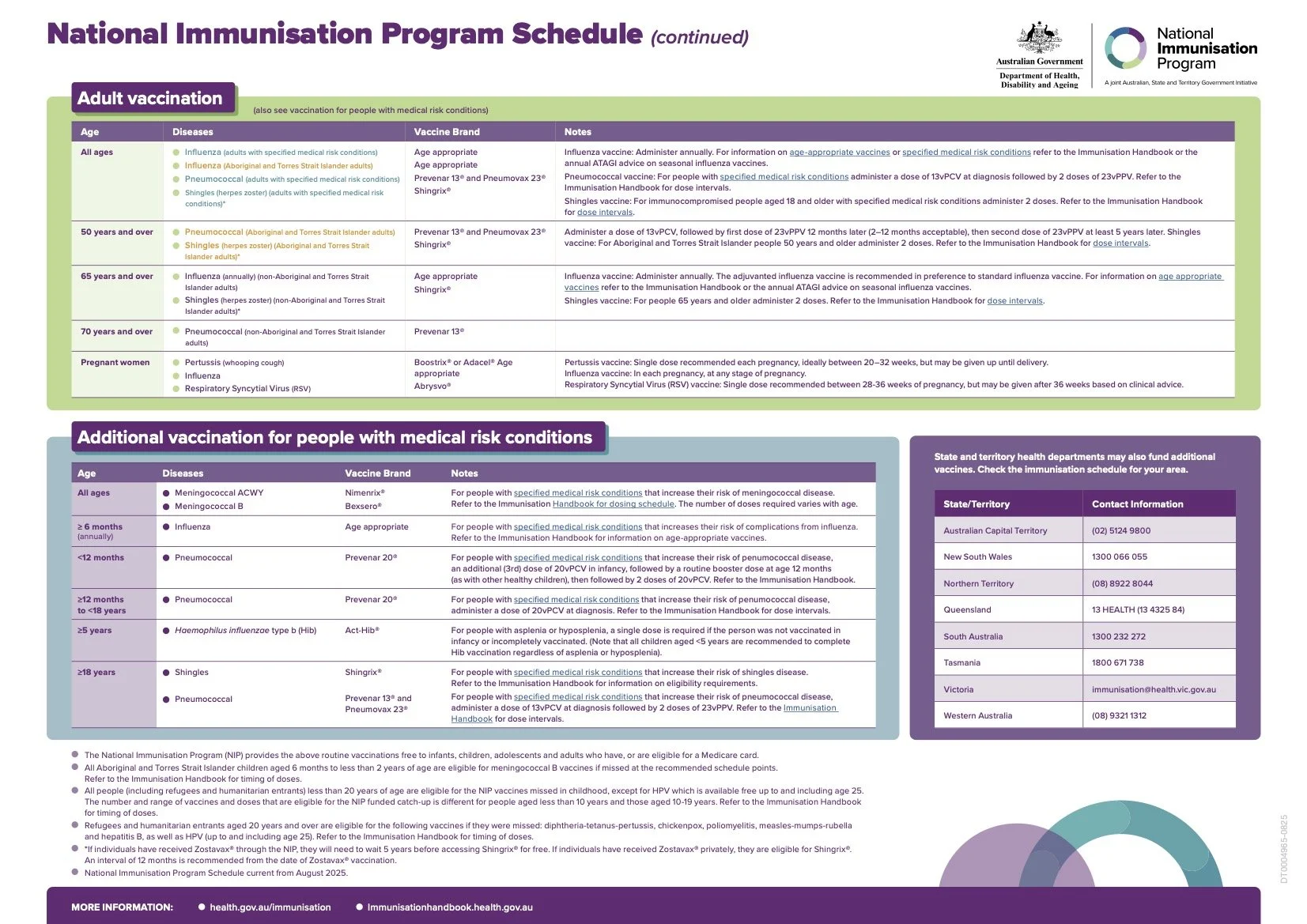
It is recommended that babies receive their first immunisation at birth for Hepatitis B. The Department of Health has established a vaccination program which is staggered throughout the growth and development of the child. The official children’s National Immunisation Program Schedule (from September 2025) is as follows:
Note: there are variables which are stipulated on the official National Immunisation Program Schedule
References